
The grand lobby of the Stanford Hospital. Photograph Copyright Bruce Damonte / Courtesy Perkins Eastman
The COVID-19 crisis has underscored the urgency of social, economic, and environmental change. In the immediacy of its threat, the pandemic has brought to light the many weaknesses and vulnerabilities in our systems, making chronic problems more acute.
The coronavirus pandemic is proof that nothing exists in a silo: everything is inextricably linked.
Erich Burkhart, FAIA, a leader of Perkins Eastman’s healthcare design practice whose background includes a Master of Science in Public Health from Columbia University, has seen the interconnection of these crises in his work more clearly than ever in recent months.
The economic, social, and environmental fallout spurred by COVID-19 has uncovered longstanding flaws in our healthcare system. Clinics and private practices are suffering financially as patients avoid in-person elective care, driving prices higher and accelerating consolidation. Chronic illnesses associated with environmental pollution, such as the smoke from the wildfires in the west, continue to rise at an alarming rate, disproportionately affecting minorities and those living in poverty, while rising medical costs also make healthcare less accessible to these populations.
We are in uncharted territory in healthcare right now, and that means the many changes in the healthcare design industry are happening in real-time. Mary-Jean Eastman, FAIA, Co-Founder and Vice-Chair of Perkins Eastman, observes, “We have been involved in several different strategies over the last six months. During the first few months of the crisis, we responded in a number of ways. As part of the Greater Hospital Association New York State Task Force, our healthcare team looked at the whole cadre of facilities in the region to understand bed surge capacity for ventilator beds.”
Perkins Eastman also joined a consortium put together by Turner Construction to build 1,100 temporary beds out of prefab structures and systems in a few weeks. We adapted this model in other areas of the country as well, planning for scenarios that would turn underutilized facilities into temporary facilities to separate COVID-19 patients from the general population.
Recovering COVID-19 patients need rehabilitative medicine, which we also need to take into consideration as we design spaces to adapt to this new reality. People recovering from the coronavirus suffer from co-morbidity — pulmonary, cardiac, and behavioral health issues. Perkins Eastman is currently working on three large ambulatory care clinics for the rehabilitation of COVID-19 patients for the Municipal Health and Hospitals Corporation. Additionally, we are consulting with several hospitals in this system to expand ICU beds and create a surgical suite for infectious patients, which will be separate from the main surgical suite.
Changes in healthcare have long been needed, and COVID-19 has only accelerated this urgency. Erich is optimistic that changes to healthcare could be for the better.
“My primary hope in all of this is that, as a nation, we will look at our healthcare system more holistically. We spend twice as much as the rest of the industrialized world on healthcare, but we get half as much out of it. We are very proud of the amazing technology breakthroughs that are part of the American healthcare system, but they only reach the people who can afford them.”
Meaningful change requires policies that support environmental, economic, and social progress. And architecture has a role to play in this progress, in the creation of spaces that can impact people and places. Erich notes, “We used to design for the convenience of physicians and nurses. Today, with the industry’s awareness of the critical link between a patients’ well-being and medical results, we need to prioritize the patient-centric experience.” Erich notes that this also means creating a humane environment for everyone involved in the patient’s care, including family, caregivers, and medical staff.
At Perkins Eastman, we embrace a holistic, human-centered, and convergent approach to design. Our healthcare projects use strategies from hospitality and retail to make staff feel more welcome, cared for, and comfortable. And crossover expertise from our work in education informs the design of spaces geared towards teaching, training, and prevention — key to empowering patients and their families to make the best decisions for their care.
“Most patients have a choice,” says Erich, “and many will make that choice based on how comfortable they are going to be in that environment.”
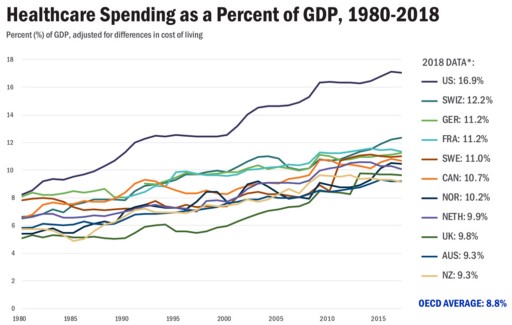
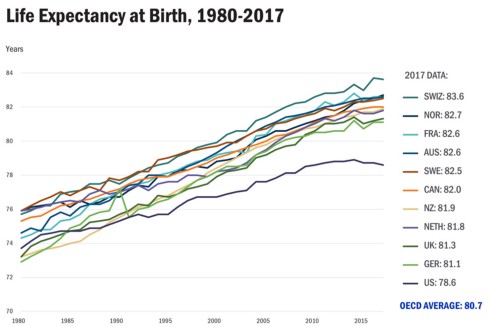
Source: Roosa Tikkanen and Melinda K. Abrams, U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes? (Commonwealth Fund, Jan. 2020).
To this end, Erich says, we can expect an increased focus on wellness, education, and preventative care. Our Wellness Center at Stanford Hospital might stand as a guide for these future models of preventative care and education. Part information center and part library, the Wellness Center provides information, guidance, and support for family members and caregivers of current or recovering patients.
“One of the reasons that the pandemic is bringing all of these issues to the forefront is that it’s an infectious disease,” Erich says. “It really encourages us to think of our health not just as individuals but as part of a community. And that’s a good thing.”
The multiple crises we are facing can only be addressed in relationship to one another; COVID-19, by its nature, demands a collective and holistic approach. To build resilience and effect positive change, we must look through and beyond COVID-19 to address the many underlying, connected issues that will shape our future.